Abstract
Sinus node dysfunction may be found not only in patient with heart disease and also as well as individuals with no previous history of heart or other disease. Unfortunately, some patients and practically healthy individuals, have not any typical (atypical) complaints or arrhythmias history. İn this study, we present a case of a 67 y. old female, practically healthy patient who developed repeatedly of different forms of Sinus node dysfunction during ambulatory Holter monitoring period. The diagnostic value of Holter monitoring in patient with asymptomatic Sinus node dysfunction episodes will be discussed here.
Full article
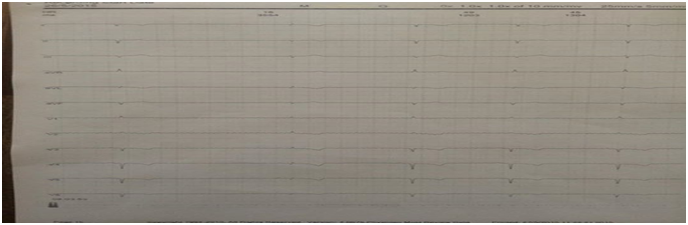
In our cases a 67 y. old female presented episode of fatigue for one year. Her past history was not for arrhythmias or other heart disorder. She had not hypertension, overweight, diabetes and hereditary predisposition. She used not alcohol and was not smoker. The patient had not received medications that can provoke sinus bradyarrhythmias (eg, beta-blockers, digoxin, angiotensin-converting enzyme inhibitors, etc). Physical examination did not suggest any significant abnormalities. Two-dimensional echocardiography revealed normal right and left ventricular size and function. Chest X-ray, blood exam and thyroid function, also were normal. The patient had no any complaints during Holter monitoring period. Ambulatory ECG monitoring showed transient atrial fibrillation during 10 second (fig.1); sinus bradycardia in night sleeping with 35 times pauses greater than 2 second and 1 time pause greater than 3.5 second (fig.2); and 178 PVC, especially 14 V – bigeminy episodes detected during continuous ECG recording. Presence of SND in our patient we associate with age. It was recommended pacemaker implantation for treatment.
Figure 1. Holter monitoring: SND – Transient atrial fibrillation
Figure 2. Holter monitoring: SND - Pauses greater than 3.5 second (Sinus arrest).
Discussion
Sinus node dysfunction (SND) also known as sinus node disease or sick sinus syndrome (SSS) is the name for a group of heart rhythm problems (arrhythmias) in which the sinus node — the heart's natural pacemaker — doesn't work properly. Some authors believe that, SND is referred to as sick sinus syndrome when it is accompanied by symptoms such as dizziness or syncope. The sinus node is an area of specialized cells in the upper right chamber of the heart that controls the rhythm of human heart. Normally, the sinus node produces a steady pace of regular electrical impulses. In SND, these signals are abnormally paced. A person with SND may have heart rhythms that are too fast, too slow, punctuated by long pauses — or an alternating combination of all of these rhythm problems (1, 2).
The disorders that characterize SND include sinus bradycardia - the heart beats very slowly, less than 60 beats per minute; sinus arrest or sinus pause is defined as absence of sinus P waves on the ECG for more than 2 seconds due to a lack of sinus nodal pacemaker activity. A sinus pause of 2 seconds is not unusual in a healthy person. However, a sinus pause of more than 3 seconds is very uncommon except under certain conditions, such as sleep apnea, hypervagotonia state, or seizure activity; sinoatrial block - the sinus node impulse is blocked fromreaching the atria, the two upper chambers of the heart and tachycardia-bradycardia (or tachy-brady) syndrome. In tachy-brady syndrome, the heart sometimes beats too quickly (tachy) and sometimes beats too slowly (brady). Types of tachycardias include atrial fibrillation, atrial flutter and supraventricular tachycardia. (3, 4)
SND may be caused by a number of factors, including damage or scarring of the heart’s electric system, caused by a disease or other health condition; scar tissue from a past heart surgery; certain medications, such as calcium channel blockers or beta blockers used to treat high blood pressure, and other conditions; the breakdown of heart muscle due to age, which is the most common risk factor. SND may be also as familial (5).
When SND is mild, patients are usually asymptomatic. As SND becomes more severe, patients may develop symptoms due to organ hypoperfusion and pulse irregularity. Such symptoms include the following: fatigue, dizziness, confusion, fall, syncope, angina, heart failure symptoms and palpitations (6).
Currently, no medications are routinely used to treat symptomatic SND. If the patient is receiving medications that can provoke sinus bradyarrhythmias (eg, beta-blockers, digoxin, etc.inhibitors), the medications should be stopped if possible. Acute treatment consists of atropine (0.04 mg/kg intravenously every 2-4 h) and/or isoproterenol (0.05-0.5 mcg/kg/min intravenously). A transvenous temporary pacemaker sometimes is required despite medical therapy. In patients with tachy-brady syndrome, the tachyarrhythmias may be controlled with digoxin, propranolol, or quinidine. However, these patients should be monitored closely with frequent Holter monitoring to ensure that the bradyarrhythmias are not exacerbated or causing symptoms (eg, dizziness, syncope, CHF); if this is the case, permanent pacemaker therapy is also required.
Conclusion:
Traditionally, ambulatory monitoring has been used to determine the cause of palpitations and syncope and, to a lesser degree, to identify ventricular ectopy or nonsustained ventricular tachycardia in patients at potential risk for sudden cardiac death.
Sinus bradycardia or Sinus arrhythmia In some cases may be found in asymptomatic and practically healthy old patents during resting (short time) ECG. In these patients life threatening types of SND may be detected only during long time ECG recording. These patients also have potential risk for sudden cardiac death. For this reason, Holter monitoring is mandatory for correct diagnosis to determine the different forms of SND in such patients
Figures

Keywords
References
1. V. Adan, and L. CrownD., Am Fam Physician. 2003 Apr 15;67(8):1725-1732.
2. Mangrum JM, DiMarco JP.The evaluation and management of bradycardia. N Engl J Med. 2000; 342:703–9.
3. Olgin JE, Zipes DP. Specific arrhythmias: Diagnosis and treatment. In RO Bonow et al., eds., Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine, 9th ed., vol. 1, pp. 771-824. 2012 Philadelphia: Saunders.
4. Vijayaraman P, Ellenbogen KA. Bradyarrhythmias andpacemakers. In V Fuster et al., eds., Hurst's The Heart, 13th ed., pp. 1025-1057. 2011. New York: McGraw-Hill Medical.
5. Olgin JE, Zipes DP. In: Specific arrhythmias: diagnosis and treatment. In: Bonow RO, Mann DL, Zipes DP, Libby P, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 9th ed. St. Louis, Mo: WB Saunders; 2011:chap. 39.
6. Zimetbaum P. Cardiac arrhythmias with supraventricular origin. In: Goldman L, Schafer AI, eds. Cecil Medicine .24th ed. Philadelphia, Pa: Saunders Elsevier; 2011:chap 64.
Article Info:
Publication history
Published: 31.May.2016
Copyright
© 2013-2025. Azerbaijan Society of Cardiology. Published by "Uptodate in Medicine" health sciences publishing. All rights reserved.Related Articles
ST-segment depression with ST-segment elevation in patient diagnosed by Holter monitoring
Viewed: 745