Abstrakt
Metabolik sindrom müasir təbabətin əsas tibbi-sosial problemlərindən biridir. Bu qrup xəstələrdə metabolik dəyişikliyi olmayan şəxslərlə müqayisədə şəkərli diabetin və ürək-damar ağırlaşmalarının inkişaf riski 2-3 dəfə çoxdur. Populyasiyada metabolik sindromun yayılmasının öyrənilməsi üzrə damar xəstəliklərinin profilaktika konsepsiyasının hazırlanmasının və həyata keçirilməsinin əsasını təşkil edir. İlk dəfə olaraq Rusiyanın Çeboksarı şəhərində 30-69 yaşda olan əhali arasında epidemioloji tədqiqat aparılmışdır. Müəyyən edilmişdir ki, bu şəhərin 30%-ə qədər əhalisində metobolik sindrom var. Bütövlükdə sosial və davranış faktorları metabolik sindromun yayılmasında böyük rol oynayır. Odur ki, bu yüksək aterogen vəziyyətin diaqnostik alqoritminin hazırlanmasında bütün bunlar nəzərə alınmalıdır.
Əsas mətn
One of the important medical and social peculiarities of metabolic syndrome (MS) is its prevalence in population, and in particular among adult population [1].
Epidemiological studies are done to estimate prevalence one or another disease or disorder. They allow revealing a wide range of regularities, including age-related and gender-related features, social, economical and ethnic factors impact. These data are of outmost importance for the disease diagnostic and prevention [2].
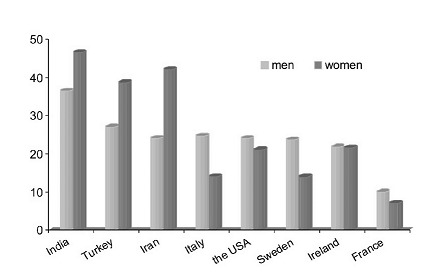
In the 1990s, there were few data concerning MS prevalence, since insulin resistance (IR) was considered an integral part of MS and glucose clamp method was a laborious and costly diagnostic procedure. One of the first epidemiological studies is San Antonio Heart Study; its results provide the basis for syndrome X concept. According to the study, 25% of adult population sample has IR without clinical manifestations [3]. Another study done in two Finland regions demonstrated that all MS components occurred in 5% of males and in 8% of females. Furthermore, MS had clear correlation with age, insulin level and obesity extent. It is worth mentioning that cut-off points of triglycerides and BP were rather high in this study [4].
Publication of the new WHO criteria in 1998 (as well its modified EGIR version) and the USA NCEP ATP III in 2001 stimulated to large-scale studies in many countries and ethnic groups. However, use of different criteria (NCEP ATP III criteria in general) makes difficult the standardization of obtained results. Currently, the data of more than 20 epidemiological studies on 5 continents are published. They allow to evaluate the global tendency of MS distribution worldwide [1,6].
The lowest prevalence of MS was registered in China (Fig.1). In Beijing study, MS was found in 10% of urban population and in 20% of people over 50. It is estimated that 90 million Chinese citizens suffer from MS [7].
In http://multitran.ru/c/m.exe?a=110&t=3267733_2_1&sc=517West European countries, MS without T2DM occurs in 10-15% of adult population and in 20% of elderly age groups [1, 8]. In the Australian AusDiab study three types of criteria were applied (WHO, EGIR, NCEP ATP III). MS was found in 16-20% of patients over 35.
A collaborate epidemiological study was done in five Mediterranean countries, which detected the most common version of MS – combination of hypertension, low level of HDL-Chttp://multitran.ru/c/m.exe?a=110&t=2588980_2_1&sc=8 and abdominal obesity (AO). Total 27% of patients in the 20 to 74 age brackets have its different variants. The similar tendency is registered in Turkey: 27% of males and 38.6% of females over 35 with low level of HDL-C and high level of LDL-C suffer from MS. It is of interest that in this sample coronary heart disease (CHD) occurred in 50% of patients with MS [9].
The largest study was done in the USA. The average prevalence of MS was 24%. However in several groups (obese people, 60-69 age group, postmenopausal females, Hispanics) this index increases to 43-56% [10]. It is estimated that about 47 million Americans have MS.
On the first International Congress on Prediabetes and the MS (April 2005, Berlin) Indian scientist A. Ramachandran reported results of an epidemiological study among Indian http://multitran.ru/c/m.exe?a=110&t=92383_2_1&sc=0urban population. The highest (41%) prevalence of MS in India occurs in the 20-75 age brackets [11]. It is known that IR and type 2 diabetes mellitus (T2DM) are widely spread in http://multitran.ru/c/m.exe?a=110&t=4698870_2_1&sc=668South Asia population.
In the post-socialist countries, including Russia, almost no large-scale studies on MS was done. It is probably associated with funding constraints [12].
In the literature, we found the results of the Poland study indicating that average 25-35% of urban population had the main components of MS [13].
The first Russian epidemiological study results of metabolic syndrome detection
In 2007-2009 National Research Center for Preventive Medicine and Ministry of Health of http://multitran.ru/c/m.exe?a=110&t=1023435_2_1&sc=291 the http://multitran.ru/c/m.exe?a=110&t=4073096_2_1&sc=72Chuvash Republic (agreement №01/01 – 1027 from 22.11.2005) did a population study to detect MS in random sample of adults at the town of Cheboksary.
Sampling
The research team (30 http://multitran.ru/c/m.exe?a=110&t=3561390_2_1&sc=8primary care physicians and general practitioners) was formed with a http://multitran.ru/c/m.exe?a=110&t=300602_2_1&sc=8random sampling technique. The study design was developed in National Research Center for Preventive Medicine in partnership with A. Deev, http://multitran.ru/c/m.exe?a=110&t=290789_2_1&sc=8biostatistics laboratory director.
According to the protocol, 60 respondents from each of the 30 http://multitran.ru/c/m.exe?a=110&t=343641_2_1&sc=8health care regions (1800 persons in total, 749 males and 1051 females at the age of 30-69) randomly selected. Research response accounted 88.7% in general.
At the first stage, 1718 persons filled in a questionnaire, which included social and demographic data, family history, http://multitran.ru/c/m.exe?a=110&t=1921377_2_1&sc=37smoking status, http://multitran.ru/c/m.exe?a=110&t=3745733_2_1&sc=107alcohol consumption, http://multitran.ru/c/m.exe?a=110&t=4601786_2_1&sc=126physical activity level, nutrition behavior, questionnaire for detection of stable anginahttp://multitran.ru/c/m.exe?t=2572214_2_1, psychological and diabetic status, hypertension course and concomitant diseases survey, taking medicines. For different reasons 148 respondents (8,7%) did not participate in the further instrumental and biochemical tests.
Clinical-instrumental tests
The anthropometric examination included waist circumference measurements, body mass and height measurement, http://multitran.ru/c/m.exe?t=4007078_2_1BMI calculation.
The office BP measurement was performed twice in the resting sitting position with a 5-minute interval with accuracy of 2 mm Hg. The mean value of http://multitran.ru/c/m.exe?a=110&t=3067706_2_1&sc=517two measurements was taken for analysis. Heart rate data were also included in the questionnaire.
All respondents underwent 12-lead ECG at rest. ECG was interpreted according to the special scheme, which was developed for this study using the Minnesota code (the USA).
CHD was diagnosed on the basis of http://multitran.ru/c/m.exe?a=110&t=46338_2_1&sc=8history analysis, http://multitran.ru/c/m.exe?a=110&t=46338_2_1&sc=8physical and instrumental examination, including the standard WHO questionnaire on exertional angina detection and ECG-proved old myocardial infarction (Minnesota code).
Laboratory tests
The tests were done in the laboratory of the Republican cardiological clinic of Ministry of Public Health and Social Development of Chuvashia in Cheboksary.
Blood samples were taken in the morning from median cubital vein in vacutainers or test tubes after 12-hour fasting with minimal venous occlusion.
Total cholesterol, triglycerides, HDL-C (mmol/L) in serum was determined by enzyme sets Human on biochemical automatic autoanalyzer ALCYON 160 (serial number 14161416) photocolorimetric method by end point CHOD – PAP (HUMAN reagents). LDL-C were calculated by Friedwald W.T. (1982) formula: LDL-C(mmol/l)= cholesterol – (triglycerides/2,2 + HDL-C).
Oral glucose tolerance test (OGTT) was done after 8-12 hour night fasting. After blood sampling, the respondents drank 75 g of glucose dissolved in 250-300 ml of water less than in 5 minutes. The blood sampling was performed twice with a 2-hour interval. Glucose concentration in venous serum was estimated by glucose oxidase test on photometer KFK-3.
Total cardiovascular risk was evaluated by European scale SCORE including the following parameters: age, sex, smoking status, systolic blood pressure (SBP) level and total cholesterol. Total risk < 1% was considered to be low risk, 1 - 4% - medium, 5-10% - high risk, > 10% - very high.
Two types of criteria were used to define MS: the NCEP ATP III (2001) and IDF (2005) definitions.
Metabolic syndrome prevalence in Russian population
MS, defined by NCEP ATP III criteria, was revealed in 314 patients (20.6%) among adults in a city of Volga Federal district (Fig.2).
226 females (28,3% of the total number of females) and 88 males suffered from MS (14,2% of the total number of males), the difference is significant (p<.0001).
According to the IDF criteria, 28,5% of respondents (n=447) have MS. It is more statistically significant (p<.0001) in comparison with MS diagnosed using NCEP ATP III.
MS 2 times more often occurs in females 35,5% (n=337) than in males17,8% (n=110), (p<.0001).
Thereby, MS diagnosed using the IDF criteria demonstrates upward tendency in the Russian population. Dr. E.S. Ford’s analysis, which was made in the Centre for Disease Control and Prevention in the USA among people over 20 years using American Heart Association criteria, revealed MS in 35,2% of cases (34,8% among males and 35,5% among females) [10]. Whereas the little difference was found using the modified IDF criteria (presence of three of five components): total 40.1%, 41,9% in males and 38,3% in females.
In this study, the majority of patients with MS met criteria NCEP ATP III and IDF. However 39.4% (n=176) of patients with MS diagnosed by the IDF criteria, did not meet the ATP III criteria. At the same time, 13.4% of patients with MS diagnosed by NCEP ATP III criteria were not included in the group of patients with MS, diagnosed by the IDF criteria.
Later in the study, we used criteria NCEP ATP III to evaluate MS associations with different social factors, and also to determine its clinical characteristics.
Age-dependent characteristics of metabolic syndrome prevalence
The analysis of MS prevalence in males as well as in females in different age groups shows that the MS prevalence grows with age. MS is diagnosed in 3.2% in males of 30-39, in the 40-49 and 50-59 age groups this rate triples to 12.2% (p<.02 compared with males of 40-49) and 14.6% (p<.004 compared with the 50-59 age group) respectively. In elderly age group (60-69 year old male) every fifth male had MS (22.6%), that is significantly more often in comparison with the 30-39 and 40-49 age groups (p<.001 and p<.03, respectively). The same pattern is typical for females. MS is diagnosed in 5% of females of 30-39; this rate grows up to 17% in the 40-49 age groups. In the 50-59 and 60-69 age groups, every third female has MS – 30.8% and 36.7% respectively, which is statistically significant compared with the age groups of 30-39 and 40-49 (Table 1).
The analysis of gender characteristics of MS prevalence shows, that in general it is 40% more frequent in females, which is most evident in 2 age groups: 50-59 and 60-69 years old (p<.002 and p<.05 respectively), compared with males of the same age.
Social status, life style, educational background and the MS prevalence
This study analyzes the influence of wide range of social factors, life style and educational background on the MS prevalence.
Initially people of different nationalities and ethnical groups were included in the study. The majority (67.7%) of them were Chuvash, one third – Russian (29,5%) and representatives of other nationalities were less than 3%, among them Tatars, Ukrainian, Belarusians and others.
The analysis of MS prevalence in 2 main nationalities demonstrated that MS can be found in 18% of cases in Chuvash population and in 25% of Russian population (p<.05). MS is diagnosed in 12% of Chuvash males and in 19% of Russian males, which is significantly higher (p<.03). The prevalence of MS in Chuvash females is 2 times higher than in males: 22.6% and 11.7% respectively (p<.0002). The difference of MS prevalence in Russian males and females is not statistically significant (19% and 26.4% respectively).
Another potential risk factor of MS is marital status. In order to estimate prevalence of MS in people with different marital status participants were divided in 4 groups: married, single, divorced and widowers. The results of the study showed that among married people every fifth participant (20%) had MS, among single people – 14%, among divorced – 18%, and the highest prevalence of MS was registered in widowers – 28,3%. In general, the lowest frequency of MS is in the group of single participants. This can be explained by the fact, that single participants were all 30-39 years old, while every third widower had MS. Equal MS prevalence is registered for divorced and married people.
The prevalence of MS in males and females of different marital status is equal, only married females are an exception – 23.8% vs. 15% (p<.002).
There is enough data in the literature on the correlation of behavioral factors with MS. On the last World Diabetes and Prediabetes Congress the results of several studies on the role of behavioral factors in the development of MS were demonstrated. The researchers of VIVIT University (Austria) demonstrated the possible association of eating disorders with MS in people with CHD [14, 15].
In this study, we studied the association of MS prevalence with life style alteration, so we analyzed data of physical activity and diet in a random sample of adults.
According to WHO questionnaire for life style, 50.9% of participants lead a sedentary life, the prevalence of MS among them was 21.8%, while among people with normal physical activity the MS prevalence was 18%. The differences between them were not statistically significant.
Every forth participant (24%) didn’t have eating disorders, while 41% of participants had light eating disorders, 27% - mild eating disorders, 8% - severe eating disorders. Among people with no eating disorders, MS was diagnosed in 14.6% of cases, in participants with mild eating disorders – in 19.2%. There is a statistically significant increase of MS prevalence in patients with mild eating disorders – 22% (p<.02 compared to people with no eating disorders). MS prevalence is the highest in group of patients with severe eating disorders and consists 32.2%, which is significantly higher compared with patients with no eating disorders or with mild eating disorders (p<.0005 and p<.01, respectively) (Table 2).
Table 3 shows the MS prevalence in correlation with smoking status. In general prevalence of MS is reliably lower in smokers (people, smoking at least 1 cigarette per day) and makes 11.3%, compared to no-smokers – 21.6% (p<.0008) and those who stopped smoking – 24.5%, (p<.002). This tendency is clear in males. In comparison to females, MS was diagnosed reliably often in smoking and non-smoking males.
To analyze the association of MS with alcohol intake patients were divided in 2 groups depending on their alcohol consumption status: people, who drink alcohol and those, who abstain from drinking. MS is significantly more frequent in people abstaining from drinking or consuming alcohol in small doses compared with people, consuming alcohol in higher doses – 21.1% and 8.8%, respectively (p<.009).
In a random sample of adults every second participant is suffering from a medium level of stress, every forth suffered from high level of stress, while only 11% of participants experienced low stress.
Among people with low stress, about 28% have the main symptoms of MS, while in the groups with medium and high stress levels, MS is registered only in 20% and 17.5% of cases respectively (Table 4).
According to previously Russian date, one of the factors, which may influence CVD in the Russian population, is the educational background [4, 12]. In general, in a random sample of adults in Cheboksary the prevalence of MS in groups with different educational background is not significantly different. It consists 17.4% in people with higher education, 19.9% - with professional education, and 21.8% - with secondary and incomplete education. MS is diagnosed significantly more often in females with secondary education as compared to females with higher education (p<.05). When compared to males, the MS prevalence in females with professional and secondary education is higher: 22.8% vs 14.2% (p<.05) and 28.3% vs 13.6% (p<.0005), respectively (Table 6).
Does working status influence the MS incidence? To get the answer to this question, we divided the participants of the study in 2 groups: working and not working.
Figure 6 shows MS prevalence in people with different working status (males as well as females). Generally MS is twice as frequent in not working people (housewives and senior citizens constitute the majority of them) as in working people and makes 29,4% and 14,9%, respectively (p<.00001). It is important to note, that in the group of not working people housewives and senior citizens were in majority.
Conclusion
As it can be seen from the above, in a random sample of people in a town in Volga Federal District there are up to 30% of cases of MS. In general, certain social and behavioral factors can directly affect MS prevalence, which should be considered in diagnostic algorithms of this highly atherogenic condition.
Şəkillər

Açar sözlər
İstinadlar
1. Balkau B, Vernay M, Mhamdi M, Novak M, Eschwege E. The French D.E.S.I.R. study. The incidence and persistence of the NCEP (National Cholesterol Education Program) metabolic syndrome. The French D.E.S.I.R. study. Diabetes Metab. 2003 Nov; 29(5):526-32
2. Abstracts book of I International Congress on “Prediabetes” and the Metabolic Syndrome. Berlin 2005 (13-16 April).
3. Hanefeld M., Kohler C. The metabolic syndrome and its epidemiologic dimensions in historical perspective. Z Arztl Fortbild Qualitatssich. 2002 Mar; 96(3): 183-8
4. Oganov R.G. Risk factor concept as the basis of CVD prevention. Vrach.. 2001; 7: 3-6 (In Russian)
5. Haffner S. Insulin and Blood Pressure in the San Antonio Heart Study: A Review. Cardiovascular Risk Factors. 1993; 1: 18-27
6. Laakso M et al. Insulin resistance syndrome in Finland. Cardiovascular risk factors 1993; 3: 44-53
7. Jia WP, Xiang KS, Chen L et al. Epidemiological study on obesity and its comorbidities in urban Chinese older than 20 years of age in Shanghai, China. Obes Rev. 2002 (Aug); 3(3): 157-65
8. Marques-Vidal P., Mazoyer E., Bongard V., Gourdy P. Prevalence of insulin resistance syndrome in southwestern France and its relationship with inflammatory and hemostatic markers. Diabetes Care. 2002 Aug; 25(8): 1371-7
9. Onat A., Ceyhan K., Basar O. et al. Metabolic syndrome: major impact on coronary risk in a population with low cholesterol level-a prospective and cross-sectional evaluation. Atherosclerosis 2002 Dec; 165(2): 285-92
10. Ford E, Giles W, Dietz W. Prevalence of the metabolic syndrome among US adults. JAMA. 2002; 287: 356-9
11. Ramachandran A, Snehalatha C, Satyavani K, Vijay V. Metabolic syndrome in urban Asian Indian adults--a population study using modified ATP III criteria. Diabetes Res Clin Pract. 2003 Jun;60(3):199-204
12. Nikitin Y.P., Kazeka G.R., Simonova G.I. Prevalence of metabolic syndrome X in unorganized population (epidemiological study). Cardiology. 2001; 9: 37-40 (In Russian)
13. Novakovich B., Popovic M. Occurrence of the metabolic syndrome in the population of the town of Novi Sad. Med Pregl. 2001 Jan-Feb; 54 (102): 17-20
14. Kiene V., Saely C.H., Boehnel C., Drexel H. Association between physical activity and the metabolic syndrome in angiographied coronary patients. Journal of Diabetes. 2009; Vol. 1. Suppl 1: A 252
15. Kiene V., Saely C.H., Vonbank A., Woess M., Drexel H. Dietary behaviour the metabolic syndrome, and coronary atherosclerosis. Journal of Diabetes. 2009; Vol. 1. Suppl 1: A217
Məqalə barədə təfərrüatlar:
Nəşr tarixçəsi
Dərc edilib: 10.Apr.2012
Müəllif hüququ
© 2013-2025. Azərbaycan Kardiologiya Cəmiyyətinin rəsmi nəşri. Jurnal "Uptodate in Medicine" tibb nəşriyyatı tərəfindən dərc olunur. Bütün hüquqlar qorunur.Əlaqəli məqalələr
Baxılıb: 1091